Summary
To move from prototype to clinical validation of a medical device, it is essential to select an R&D partner that combines methodological rigour, development speed, and creativity; possesses deep expertise in the device’s critical elements along with a strong system-level perspective; and has the infrastructure, prototyping capabilities, and partner network required to provide a clear path toward production transfer.
Moving from a functional prototype to clinical validation is one of the most critical stages in medical device development.
It is at this point that technical, regulatory, and industrial risks converge—and where the choice of R&D partner becomes decisive to project success.
A strong partner does more than provide technical resources: they must be able to structure, accelerate, and secure the development pathway all the way to the clinic. Below are the key criteria to guide the right choice.
Ensure Alignment with Your Development Roadmap
Every medical device follows a specific development roadmap influenced by:
- the device class,
- regulatory requirements,
- funding milestones,
- clinical timelines.
A relevant R&D partner must demonstrate:
- methodological rigour aligned with medical-sector requirements,
- development speed suited to your market-entry constraints,
- creativity and innovation capacity to address unexpected technical challenges.
The objective is not only to achieve technical performance, but to do so at the right pace and with controlled risk.
Ensure Deep Expertise and a Strong System-Level Vision
Clinical validation rarely depends on a single technical element. It relies on the interaction between:
- the device’s critical components (optics, electronics, mechanics, software),
- the overall system architecture,
- manufacturing and assembly methods.
A strong centre of expertise must offer:
- deep experience with the key technological elements of your device,
- a system-level perspective capable of managing design, integration, and prototyping activities end to end.
This holistic approach reduces the risk of late-stage re-engineering, which is often costly and time-consuming as clinical trials approach.
Assess Infrastructure and Prototyping Capabilities
Moving from prototype to clinical validation requires high standards of:
- precision,
- repeatability,
- traceability,
- documentation.
It is therefore essential that the R&D partner has:
- the infrastructure required to develop advanced prototypes,
- in-house manufacturing and assembly capabilities,
- a network of qualified partners to complement missing expertise.
An integrated environment accelerates iterations and increases the reliability of prototypes submitted for validation.
Require a Clear Path Toward Production Transfer
A clinically validated prototype must be industrializable. From the R&D phase onward, the partner should demonstrate:
- an understanding of higher-volume manufacturing challenges,
- the ability to anticipate cost and quality constraints,
- a clear technology transfer pathway.
Continuity between development and production is a key factor in reducing the time between clinical validation and commercialization.
Why Rely on a Recognized Centre of Expertise?
Centres of expertise supporting projects in demanding sectors such as medical devices, space, and advanced manufacturing have developed:
- proven methodologies,
- proprietary tools,
- a strong culture of technological risk management.
INO has supported companies for decades in the development, prototyping, and transfer of medical technologies.
This experience enables a structured approach—from early functional iterations through to clinical validation and production.
Conclusion
When selecting an R&D partner or centre of expertise to support you from prototype to clinical validation, ensure that they:
- are aligned with your development roadmap,
- possess deep expertise in critical elements and a strong system-level vision,
- have the required infrastructure and prototyping capabilities,
- offer a clear path toward production transfer.
This strategic choice can make the difference between a promising prototype—and a medical device truly ready for the clinic.

Discover how to accelerate the development of optical medical devices through an integrated partnership in our reference guide.
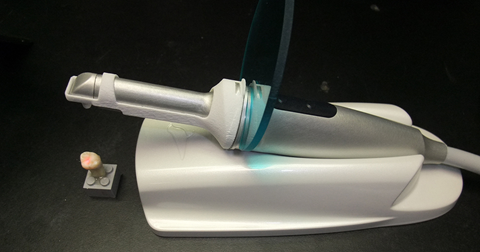
Discover how INO helped Quantum Dental Technologies Inc. deliver a better solution to its customers for the early detection of dental caries.

